Eye Conditions
What Is Glaucoma?
Glaucoma Surgery
Glaucoma is a complex disease. It is often referred to as “the sneak thief of sight” because the symptoms are not noted until late within the disease process. More than 2.2 million Americans over the age of 40 have open-angle glaucoma, the most common form of glaucoma. At least half don’t even know they have it. Once vision is lost, it can not be restored. Glaucoma is one of the leading causes of blindness in the United States. Glaucoma causes damage to the optic nerve leads to progressive, irreversible vision loss.
Glaucoma is a disease in which damage to the optic nerve leads to progressive, irreversible vision loss.
Increase in intraocular pressure caused by malfunction of the eye’s drainage system or by malformation causes irreversible damage of retina fibers layers results in permanent, progressive vision loss. As the damage occurs in the optic nerve, you begin to lose patches of vision, usually side or peripheral vision. This is eventually followed by central vision. Therefore, by the time a patient is aware of vision loss, the disease is usually quite advanced.
Regular eye exams, early detection and treatment are the keys to preventing permanent optic nerve damage and permanent blindness form glaucoma.
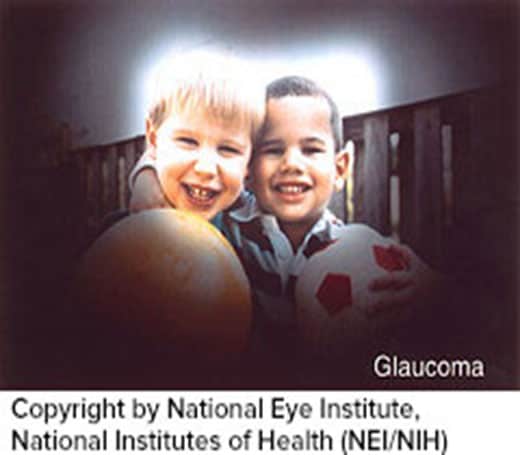
Most people who have glaucoma feel fine and do not notice a change in their vision at first because the initial loss of vision is of side or peripheral vision, and the visual acuity or sharpnessof vision is maintained until late in the disease. This is particularly true for those who have open-angle Glaucoma.
By the time a patient is aware of vision loss, the disease is usually quite advanced. Without proper treatment, glaucoma can lead to blindness. The good news is that with regular eye exams, early detection, and treatment, you can preserve your vision.

What Are the Types of Glaucoma?
There are two main types of glaucoma:
- Open-angle glaucoma. Also called wide-angle glaucoma, it is the most common type of glaucoma. The structures of the eye appear normal, but fluid in the eye does not flow properly through the drain of the eye, called the trabecular meshwork. Typically, open-angle glaucoma has no symptoms in its early stages, and vision remains normal. As the optic nerve becomes more damaged, blank spots begin to appear in your field of vision. You normally would not notice these blank spots in your day-to-day activities until the optic nerve is significantly damaged and these spots become large. If all the optic nerve fibers die, blindness results.
- Angle-closure glaucoma. Also called acute or chronic angle-closure or narrow-angle glaucoma, this type of glaucoma is less common but can cause a sudden build up of pressure in the eye. Drainage may be poor because the angle between the iris and the cornea (where a drainage channel for the eye is located) is too narrow. Since the fluid cannot exit the eye properly, pressure inside the eye builds rapidly and causes an acute closed-angle attack. Symptoms may include; blurred vision, severe eye.
Pain, headache, rainbow-colored halos around lights, nausea build and vomiting. THIS IS A TRUE EMERGENCY. If you have any of these symptoms, call Dr. Pacuraru immediately. Unless this type of glaucoma is treated quickly, blindness can result. Two-thirds of those with closed-angle glaucoma develop it slowly without and symptoms prior to an attack.
Optic Nerve Damage
In open-angle glaucoma, the angle in your eye where the iris meets the cornea is as wide and open as it should be, but the eye’s drainage canals become clogged over time, causing an increase in internal eye pressure and subsequent damage to the optic nerve. It is the most common type of glaucoma, affecting about four million Americans, many of whom do not know they have the disease.
What Causes Glaucoma?
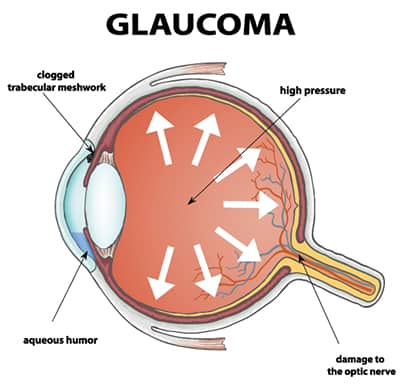
In a healthy eye, aqueous fluid (a watery fluid) is produced by the cilliary body. It flows through the pupil and behind the clear cornea. Finally it drains away through the trabecular meshwork into the bloodstream.
In glaucoma patients, fluid can’t drain properly due to an inefficient drainage system. So, there is no place for excess fluid to go and the pressure inside the eye builds up.
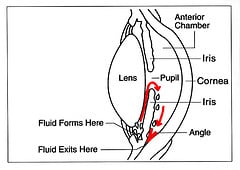
Fluid pressure within the eye increases pushing against the optic nerve and causing damage. Just as a sink drain backs up with water if it were closed up, the pressure inside the eye build up because there is no place for the excess fluid to go.
For other patients, glaucoma damages the optic nerve without increased pressure. These patients may be unusually sensitive to normal levels of pressure. Their glaucoma is often related to decreased blood flow in the eye.
Increased RiskDuring your exam, Dr. Pacuraru takes into consideration many factors in determining your risk for glaucoma. Some risks factors include:
-
- Family History of the Disease
- Age
- Elevated eye pressure
- African or Hispanic ancestry
- Asian
- Alaskan Natives
- Farsighted or nearsightedness
- Past eye injuries
- Thinner central corneal thickness
- Health problems including diabetes, migraine headaches, and poor circulation
- Pre-existing thinning of the optic nerve
- Steroid users
How is glaucoma detected and diagnosed?
Regular eye exams are the best way to detect glaucoma. During your glaucoma evaluation with Dr. Pacuraru, she may preform some of the following testing:
Measuring your intraocular pressure (tonometry) -Inspect the drainage angle of your eye (gonioscopy) -Evaluate whether or not there is any optic nerve damage (ophthalmoscopy) -Test the peripheral vision of each eye (visual field)
Photographing the optic nerve through Fundus Photography -Perform HRT/OCT to scan and measure the thickness of nerve fiber layers in the retina -Pachymetry- Thickness of the cornea.
How is Glaucoma Controlled and Diagnosed?
It is important to understand that there is no cure for Glaucoma. All treatments are aimed at controlling the disease. Once vision is lost from glaucoma it does not come back.
Medications
Glaucoma is usually controlled with eye drops taken daily. These medications work by lowering the eye pressure either by decreasing the amount of aqueous fluid produced within the eye or by improving flow through the drainage angle.
Never change or stop taking your medications without consulting Dr. Pacuraru. If you are about to run out of your medication, please ask for a refill at your next visit or call our office.
Glaucoma medications can preserve your vision, but they may also produce side effects. You should notify your ophthalmologist if you think you may be experiencing side effects.
Some eye drops may cause:
- Stinging or itching
- Red eye or redness of the skin surrounding the eyes
- Changes in pulse and heartbeat
- Changes in energy level
- Shortness of breath (especially with asthma and emphysema)
- Dry Mouth
- Eyelash growth
- Blurred vision
- Change in eye color
If you experience any shortness of breath, swelling, or pain associated with your medication. Please contact our office.
Other Treatments for Glaucoma
Laser Surgery
Laser surgery treatment maybe recommended for different types of glaucoma.
Dr. Pacuraru and the staff at Abilene Premier Eye Care are proud to offer the following:
SLT- Selective Laser Trabeculoplasty is an in office treatment that may be an option for patients with open-angle glaucoma who have difficulty maintaining consistent results with drops and medication. This procedure uses a neodymium YAG laser to focus light energy on the internal drainage channel of the eye. SLT targets the pigmented (melanin-containing) cells in the trabecular meshwork using a very short application of light. Because SLT uses a low amount of energy the surrounding tissue is not damaged. The treatment allows the drain to work more efficiently.
The laser stimulates the body’s natural healing response, improving fluid flow more efficiently. The procedure causes less scarring since the laser energy only interacts with pigmented cells. This procedure lowers the pressure more than 80 percent of the time. After SLT, your eye pressure may increase over time. By five years up to half of the people treated with SLT experience a rise in eye pressure. Your doctor will need to continue to monitor your eye pressure and can repeat the SLT treatment if needed.
In closed-angle glaucoma, a laser can be used in-office to create a hole in the iris. This procedure takes only a few minutes and is called an LPI or Laser Peripheral Iridotomy.
Surgery in the Operating Room
When surgery in the operating room is required. Dr. Pacuraru is pleased to offer her patients the state-of-the-art surgical facilities at Texas Midwest Surgical Center and Hendrick Medical Center.
What is trabeculectomy surgery?
Trabeculectomy surgery creates a new drainage site to help filter internal fluid from the eye. Instead of going through the normal drainage site of the eye (the trabecular meshwork), the fluid is drained into a new “space” that is created underneath the outer covering (the conjunctiva) of the eye. This will lower the eye’s fluid pressure.
When is trabeculectomy surgery indicated?
Trabeculectomy is generally recommended for patients with glaucoma that continues to progress despite use of medications and/or lasertreatments. In some cases, trabeculectomy surgery may berecommended prior to trying medical or laser treatment. These decisions vary depending on the type of glaucoma, the stage of glaucoma, as well as other factors. Sometimes this surgery can be combined with cataract surgery.
What should I expect if I have trabeculectomy surgery?
The procedure is done under local anesthesia in the operating room. After some eye drops are put in the eye and after the eye is numbed, your eye will be cleaned. A sterile drape is put over your face and body, leavingonly your eye uncovered, to keep the operation area clean and sterile. Your eye will be held open by a “lid speculum,” so you will not blink during the surgery. Some surgeons may also give you sedating medications through an IV (intravenous) line to keep you completely comfortable. After the surgery is over, a patch and shield will be placed over your eye. This will be removed the day after surgery on your first post-operative visit. You should expect to be seen quite frequently by your surgeon until the eye completely heals. For many people, this may take up to two or three months. During this time, you will be taking frequent and multiple eye drops. You may also need removal of sutures, a laser procedure to cut some sutures, injections of supplemental medications, or other procedures to guide the healing process toward the best result. You will also be restricted from strenuous activities during the healing process. In general, post-operative care will vary from patient to patient.
Laser Cyclophotocoagulation
Cyclophotocoagulation is generally used to treat advanced or aggressive open-angle glaucoma. It is usually used after other treatments have proven unsuccessful. Dr. Pacuraru will perform the treatment at Texas Midwest Surgery Center
In open-angle glaucoma, the eye’s aqueous humor (the clear liquid that circulates inside the front portion of the eye) does not drain properly. This causes pressure to build up within the eye. The medical term for this pressure is intraocular pressure. Such pressure inside the eye may damage the optic nerve and lead to vision loss. Medications, laser surgery, or other glaucoma surgeries may be used to lower and control the eye pressure.
During cyclophotocoagulation surgery, your doctor will point a laser at the white part of your eye (sclera). The laser passes through the sclera to the ciliary body, the part of the eye that makes eye fluid (aqueous humor). The laser damages parts of the ciliary body so that it will make less eye fluid, which lowers eye pressure. This surgery is usually done at a doctor’s office or outpatient surgery clinic.
The procedure is performed with local anesthesia. When the anesthetic wears off after the procedure, you may experience some pain or discomfort.
In follow-up exams after cyclophotocoagulation, Dr. Pacuraru will check for inflammation and monitor the pressure in your eye.
Shunts and Tubes Glaucoma Treatment
What is a tube shunt drainage device?
Glaucoma tube shunts are devices that are implanted in the eye to provide an artificial alternative drainage site for fluid to exit the eye. A tiny tube extends from the body of the device into the anterior chamber, which is the front part of the eye that usually drains fluid from the eye. The device allows excess fluid to drain out through the tube and be absorbed in surrounding tissues. Glaucoma tubes come in many different varieties.
When is a tube shunt procedure indicated?
Glaucoma tube shunt surgery may be needed in patients with glaucoma that is not controlled by medications and/or laser treatment. It may be needed either after failure of previous trabeculectomy surgery (or surgeries) or in certain types of glaucoma where traditional trabeculectomy surgery would almost certainly fail. Examples of such patients are those with neovascular glaucoma, and patients who have corneal transplants.
What is done during the tube shunt procedure?
Usually, a small incision is made near the top of eye underneath the conjunctiva, the thin outer covering of the eye. The body of the device lies over the top of the eye but underneath the outer covering of the eye. After the body of the device is sutured in place, the tube, which extends from the body of the device, is inserted into the eye’s anterior chamber. Although the device is sutured onto the top of the eye, it is completely covered by the eye’s white outer covering, the conjunctiva. Most, if not all, of the device will not be visible behind the upper eyelid after the surgery.
What should I expect if I have a tube shunt procedure?
The procedure is done under local anesthesia in the operating room. First, eye drops are used to numb the eye. Then, your eye will be cleaned and a sterile drape will be put over your face and body, leaving only your eye uncovered. This keeps the area of the operation clean and sterile. Your eye will be held open by a “lid speculum,” so you will not blink during the surgery. Some surgeons may also give your sedating medications through an IV (intravenous) line to keep you completely comfortable. After the surgery is over, a patch and shield will be placed over your eye. This will be removed the day after surgery on your first post-operative visit. You should expect to be seen frequently by your surgeon until the eye completely heals. For many people, this may take six to eight weeks. During this time, you will be taking frequent and multiple eye drops. The post-operative care varies greatly and may include suture removal and/or other minor procedures to maximize the outcome of the surgery. During this time, you will need to restrict yourself from strenuous activities.
Will my glaucoma be cured with the glaucoma tube device?
No. Any vision that is already lost prior to the surgery, in general, will not return. Tube shunt surgery only lowers your eye pressure. By lowering the eye pressure, the goal is to either stop or slow down your loss of vision. Sometimes this goal is not possible.
If you have questions about these or any treatments offered at Abilene Premier Eye Care. Please feel free to contact us.
